In the past few weeks, health authorities have identified an outbreak of monkeypox in more than twenty countries, including the United States. The virus, which is endemic to western and central Africa, likely spread to Europe by someone traveling from western Africa. Since then, the unprecedented spread of the disease has been primarily linked to sex between men at raves, bathhouses, and Gay Pride events.
Monkeypox can spread through large respiratory droplets and bodily fluids, typically from close or intimate contact over long periods of time. The particular strain in this outbreak is likely one of the less lethal versions, with a fatality rate of less than 1%. As of Thursday, May 26, there were nine cases of monkeypox in the US across seven states, including Massachusetts, Utah, Washington, California, Florida, Virgina, and New York.
Anyone can get and spread monkeypox. Its concentration among gay and bisexual men who have sex with other men at this point in the pandemic is due to several factors: the virus needs prolonged close contact to spread, such as sex, and gay men are more likely than other groups to have casual sex with multiple partners. They are statistically less likely to be tied down by children, and in gay culture, casual sex is not tabboo and monogamy is less common. Because of PrEP, the miracle regimen that prevents HIV infection, alongside extremely effective antiretroviral cocktails that make HIV-positive men undetectable and untransmissable, condom use has declined significantly.
Thousands of gay and bisexual men who have sex with men are in Chicago for the International Mr. Leather conference, the first since 2019 because of the pandemic, oriented around BDSM interests. Many of the participants will have casual sex.
Millions of queer people will travel to different cities for Pride Month festivities every June weekend, during which some will also have casual sex. Chicago has the biggest Pride parade in the Midwest, having attracted more than 1 million people in past years, scheduled this year for June 26.
During a May 23 press briefing, Dr. John Brooks, the chief medical epidemiologist of the Division of HIV Protection at the Centers for Disease Control and Prevention (CDC), euphemistically called the European “events that have been described where (men who have sex with men) gather” potential monkeypox super-spreading sites. “That’s another reason for us to really want to rapidly bring people’s attention to this risk so that folks are aware and they can take action appropriately.”
And the CDC reported on May 26 that there is now community spread of monkeypox in the United States, meaning that some of the people in this country known to have it do not have a history of travel to other countries with known outbreaks.
“[We are] doing the hard work of public health, the epidemiology and contact tracing, that allows us to trace chains of transmission and hopefully cut them off,” CDC Director Dr. Rochelle Walensky said in a press briefing.
Monkeypox primarily spreads through skin-to-skin contact. That it spreads through respiratory droplets does not mean that it is airborne; it is unlikely that you would get it at a grocery store. The CDC says you need to be in close contact with someone (i.e., six feet) for three hours or more for the droplets to be a risk.
The disease has about a two-week incubation period, though it can range from five to twenty-one days, between which a person is infected and can start showing symptoms. Those symptoms can include head and muscle aches, swollen lymph nodes, and fevers.
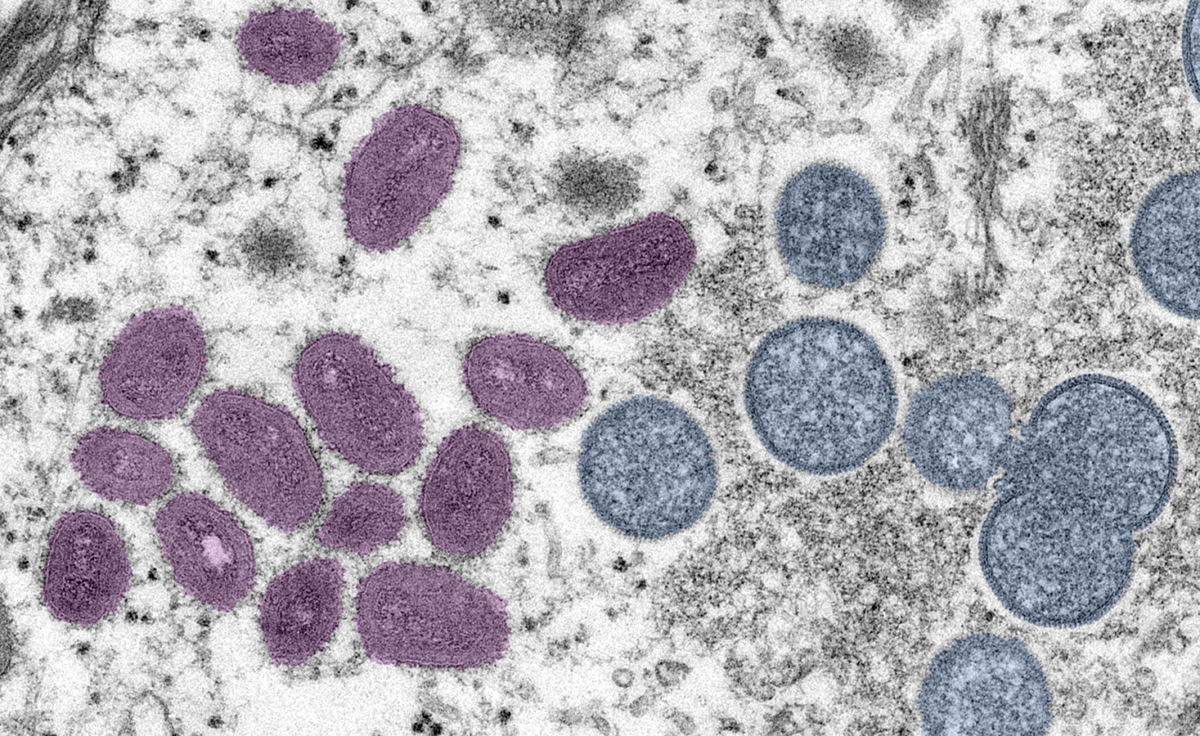
The tell-tale sign of the disease is the rash. The pox typically appear on the face before spreading to the rest of the body, bumping up, then filling with clear fluid and then pus. Then they burst and scab. Sometimes they merge to form big lesions. When they heal, the person is over the disease.
With this outbreak, however, the non-rash symptoms can be mild, and the lesions are appearing in other places: on the genitals, on and inside the anus, in the mouth and in the throat. When they present, they are fewer in number and more encrusted.
“It does infect the mucosal lining and patients are presenting with proctitis, or pain in the rectum like when they’re having a bowel movement, without necessarily visible lesions,” said Dr. Cathy Creticos, director of infectious diseases and medical director of clinical research for Howard Brown Health, Chicago’s biggest network of LGBTQ health care clinics.
Most of the lesions are outside of the area that a condom covers. (Creticos said she couldn’t say that condoms don’t reduce the risk, even though they don’t cover all the skin where rashes can be; of course, they substantially reduce the risk of STD transmission.)
People may think that if their partners don’t have open sores or a rash, it’s safe to engage in sex with them. While Creticos believes the rash must be present for skin-to-skin contact to spread the disease, she pointed out that monkeypox can still spread through respiratory droplets and bodily fluids if the other symptoms are present, such as fevers, head and muscle aches and swollen glands.
And those symptoms can be mild. Many a gay man, among other people, has chosen a good time over staying home because of a little headache.
During the past 50 years of our experience with monkeypox in Africa we’ve learned a lot about the virus, but I will say that we’re learning even more with this outbreak,” said U.S. Public Health Service Commissioned Corps Capt. Dr. Jennifer McQuiston, the CDC’s deputy director of the Division of High-Consequence Pathogens and Pathology, on a May 23 press call.
She said one of the best ways to deal with cases is to keep sick people isolated. That’s going to be hard. Again, people are infectious until the lesions are gone and the scabs fall off, though people can cover the lesions up and not have sex while they have them. Creticos said people are being asked to stay apart from others in their household and to mask up if they do come into contact (they should also not share bedding or towels), but a twenty-one-day illness is a long time to isolate.
“I don’t know how aggressive public health officials are going to be about isolating,” she said. “But the good news is that we are all very familiar with wearing masks, so if an individual with monkeypox decides to go out, first of all casual contact like going to a grocery store isn’t going to spread it, and covering up the lesions and wearing a mask seems like a very reasonable thing to do.”
While the overwhelming number of cases in this outbreak are affecting men who have sex with men, anyone can get monkeypox. Some of those men have sex with women. Bedding, clothes and towels can spread it; last week, at least three cases turned up in Europe who did not get it through household spread, Creticos said: two people in the same household as someone who had it and one health care worker.
Every medical professional has stressed that the virus can affect anyone. Brooks, the CDC HIV-prevention director, said, “If you’re feeling ill and you have a rash, it might be a good time to step back. And if you, after an event, find that you are a person who has developed some symptoms or rash that’s suspicious for possible monkeypox, seek evaluation.”
Unexplained rashes or other symptoms should result in a trip to the doctor or a sexual health clinic for those who do not have a primary care provider or health insurance. Brooks said those seeking care should tell their providers that monkeypox is being observed in other parts of the world with “a notable fraction of cases occurring among gay men.”
“Don’t hesitate to advocate for your health and inform your doctor of your concerns if you think you might have been exposed,” he said. “I want you to know that CDC is working to provide frontline health providers and public health officials with information about what the monkeypox infection looks like and how to manage the illness.”
“We’re concerned enough of the pace at which the new cases are developing worldwide that we want to raise everyone’s attention and be very vigilant so we can try to control this as quickly as possible,” he said.
Without sufficient evidence of rapid spread, he said there is no need to recommend that large gatherings be shut down.
He additionally noted that it is not a sexually transmitted disease “in a typical sense” — STDs are those like chlamydia or HIV/AIDS that solely or predominantly spread through sexual contact — but he reiterated that “it can be transmitted through sexual and intimate contact.”
On May 27, Mayor Lori Lightfoot said the Chicago Department of Public Health has “led the way” over the past two pandemic years, that it can track monkeypox, and that the city is on alert. “We’re talking about it on a regular basis, and they’re making preparations,” she said.
On May 26, CDPH Commissioner Dr. Allison Arwady said the department is closely monitoring the outbreak and that she would not be surprised to see some cases here, though she stressed that that does not mean the disease is a big problem right now. She said clinicians are calling the department, and she, too, urged people with new rashes to visit doctors, adding that she hopes they would do that in any event.
“This at this point has not been an explosive kind of outbreak. We’re communicating, but one of my bigger concerns is that people could get mistaken for syphilis. There are also diseases that present, and I don’t want people thinking that this is for-sure sexually transmitted or even entirely in this population,” she said.
The same day, Dr. Raj Panjabi, an epidemiologist who heads the White House pandemic office, said the Biden administration is prepared to face the outbreak but that “a monkeypox outbreak of this scale and scope across the world has not been seen before.”
“We shouldn’t be more surprised to see more cases reported from the U.S. in the upcoming days,” he said. “It’s actually a sign that Americans are remaining vigilant and health care providers and public health workers are doing their job.”
Walensky said the CDC has been preparing for this type of outbreak for decades, with two preventive vaccines and two antiviral treatments that can be used against orthopox (the family of viruses that includes cowpox). One is approved for adults. She said the CDC can move the regimens across the country and is indeed already moving the vaccine to states with reported cases.
Creticos, with Howard Brown, said she thinks the CDC is trying to walk a fine line between emphasizing that monkeypox is primarily being spread between gay and bisexual men who have sex with men in this outbreak and making sure people understand that this is not a “gay disease.”
“And, boy, having gone through the HIV pandemic and seeing still how it’s kind of second-fiddle to other diseases, once it becomes labeled the gay disease, it’s not important to people,” she said. “It’s kind of like ’that’s a disposable element of our population, they don’t impact my life, it’s not my problem.’”
Like Panjabi, Creticos thinks there will be “a very rapid increase in cases.” She thinks the disease has already spread.
“The incubation period is nine to 13 days,” she said. “Patients who are coming to health clinics now were infected maybe two weeks ago, so there’s clearly going to be more cases. It’s probably going to rise exponentially. The hope is that we’re going to be able to contain it, because we can identify it.”
The profoundly bad timing of this outbreak, right at the beginning of Pride Month, is a complicating factor.
“This is a community that has the strength and has demonstrated the ability to address challenges to their health by focusing on compassion and science,” Walensky said. “I urge everyone, those in public health, clinical providers and the community, to stand in solidarity with the LGBTQ community.”
Creticos noted that the scope of the disease is still limited in the U.S. at the end of May. “Probably the important thing is to know about it, to have some level of concern, and if you have suspicions or you’re worried about something, then take that extra step to try to protect yourself to get care as soon as you can as soon as something’s going on.”
It will get worse over the course of June. “Is it going to stop at 1,500? Are we going to go up to 20,000? Are we going to round out at 500? I don’t know,” Creticos said. “I think we are all uncertain.”
“Gay men became really active about trying to be proactive about their health care and demanding that their health care needs be addressed, and that there be a level of responsibility both among their population and from health care providers,” she said.
Meanwhile, there is a meningitis outbreak going on among gay and bisexual men who have sex with men in Florida right now, bad enough that the CDC and the Florida Department of Health are encouraging men who have sex with men there to get vaccinated against the disease.
Meningitis causes swelling of the membranes around the brain and spinal cord; symptoms are headaches, fevers and stiff necks, and it can be fatal. But the bacteria that causes it typically sits in the throat and doesn’t do anything; Creticos said up to six percent of people can carry it. People come into contact with it through kissing, sharing utensils, etc. But sometimes there’s a more infectious strain that gets established in the population, and authorities vaccinate everyone who is at risk and treat close contacts with a short case of antibiotics when that happens.
“It’s nothing special about gay men,” Creticos said, noting that outbreaks occur among military recruits, college students living in dormitories and pilgrims doing the hajj in Mecca, Saudi Arabia: “Wherever you have congregations of very intense physical interactions, especially where you have people either eating and drinking together or kissing.”
Even though the outbreak is in Florida, contacts of infected people who become colonized with the same strain can and have come north and begun infecting sexual partners. Howard Brown is actively vaccinating anyone traveling to Florida—it’s a one-dose sequence for most people and a two-dose sequence two months apart for HIV-positive people. The vaccines are good for five years.
“It’s a very safe vaccine. It doesn’t cause any side effects,” said Creticos. “You can give it to people who are immunocompromised. It’s not new technology, like mRNA (which the Pfizer-BioNTech and Moderna COVID-19 vaccines use). There’s really no reason why people should have concerns about taking the vaccine.”
She said there’s no reason why men who have sex with men in Illinois shouldn’t get vaccinated with the MenACWY vaccine.
Asked about the meningitis outbreak in Florida, Arwady said Chicago has a good surveillance system in place for the disease and is used to responding to it. She does not have a high level of concern at this point, but if people are worried, she encourages people to learn about the symptoms and if symptomatic, to see a health care provider.
Ald. Maria Hadden (49th), the lesbian City Council member from Rogers Park, has sprung into action in response to the monkeypox threat, including the council’s LGBT Caucus on messaging to the city and CDPH about the outbreak and getting information out about the disease on her social media pages and to LGBTQ-serving businesses on the North Side.
Ald. Raymond Lopez (15th), the only openly gay alderperson on the South Side, noted Arwady’s past CDPH work with controlling Chicagoland’s summer 2015 meningitis outbreak among men who have sex with men. The Tribune reported that Black men were disproportionately affected by that outbreak; to counter it, the CDPH did mass vaccination events at the Center on Halsted in Lakeview, 3656 N. Halsted St., Jackson Park and the rocks at Montrose Beach during that year’s Pride parade.
Lopez noted that CDPH utilized apps like Grindr, the omnipresent gay social networking and hookup app, to do outreach against the meningitis outbreak. “Monkeypox isn’t technically an STD, but it’s a virus of proximity,” he said. “That is something that we should again look at reactivating on a broader scale, but specifically as it relates to the LGBTQ-plus community, making sure that we are engaging with these apps to identify who are the spreaders of this and who are most in danger of contracting it.”
“I’m hopeful that many of the same policies that we used last time to address meningitis can be activated and incorporated in preparation for the spread of monkeypox, particularly amongst LGBTQ people.”
Dr. Anu Hazra, an assistant professor of infectious diseases at the University of Chicago Pritzker School of Medicine, said monkeypox’s long incubation period between infection and someone showing symptoms, when the person is not infectious, allows authorities a lot of time to trace contacts and tell them they have been exposed. Those contacts can be instructed to avoid contact until they’re out of their own incubation period, when it will be known whether they’ve gotten monkeypox themselves or not.
Hazra said information needs to get to people who need it in a non-stigmatizing way. “The last thing you want to do is stigmatize this illness as a gay illness or an illness of promiscuous people, and then people will be afraid to come forward with symptoms because they don’t want to be labeled as such either,” he said.
“Right now in this initial part of this outbreak, what we’ve been seeing is that it’s spreading in sexual networks, and specifically sexual networks of gay and bisexual men who have sex [with men],” he said. “If you are in that community, population or identify as someone who has sex with men or has sex with more than one partner who is a male, you should think about this. You should know about this. You should know what to look out for, specifically anal and genital symptoms. And you should know where to go to get testing done if that happens.”
Aaron Gettinger is a staff writer at the Hyde Park Herald. He last wrote for the Weekly about the 2019 aldermanic election in the 20th Ward.