Masks: why they work
- When you breathe, talk, sing, cough, or sneeze, you release respiratory droplets into the space around you. If you’re infected with COVID-19, even if you don’t have symptoms, you will be releasing droplets with COVID-19.
- Covering your mouth and nose with a mask reduces the spread of respiratory droplets, which can reduce community spread of COVID-19. Transmission of SARS was reduced by seventy percent with consistent mask wearing, and one early study of COVID-19 transmission. suggested that face mask use before developing symptoms prevented infecting close contacts by seventy-nine percent.
- New evidence suggests wearing masks can reduce how much of the virus that causes COVID-19 you’re exposed to, which may reduce your chances of developing symptomatic illness.
How to wear a mask
- Wash your hands before and after handling the mask.
- Try to touch only the ear bands or ties on your mask when putting it on and taking it off.
- Make sure the mask fits as snugly as possible over your nose, mouth, and chin.
- Make sure you can breathe and talk comfortably in your mask.
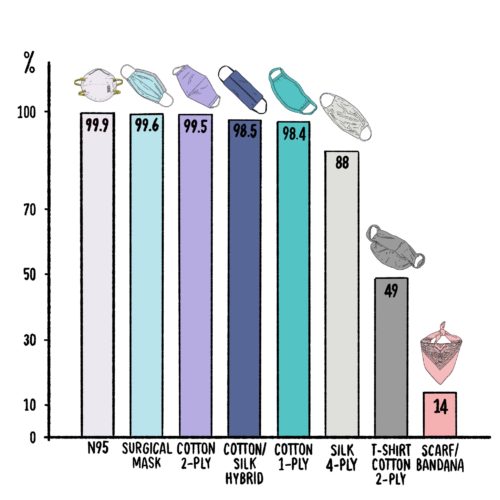
Face coverings ranked
- Fitted N95 (99.9 percent filtration efficiency*)
- Fitted Surgical Mask (99.6 percent)
- Cotton (2 layers, 600 thread count) (99.5 percent)
- Cotton/Silk hybrid with no gaps (98.5 percent
- Cotton (1 layer, 600 thread count) (98.4 percent)
- Silk (4 layers) (88%)
- T-shirt Cotton (2 layers) (49%)
- Scarf/Bandana (14%)
- No Mask
- *based on filtration percentages for particles >300 nm in size. Respiratory droplets are around 5000 nm in size; it is still unclear if COVID-19 can also disperse through aerosols (see COVID: Airborne or Droplet? below), which are much smaller in size and for which filtration efficiencies are slightly lower.
- Vacuum bags and furnace filters have also been examined as possible materials for homemade masks, but these have the possibility of containing small glass particles that are dangerous if inhaled.
Important mask facts

-
- Wearing any mask helps limit spread.
- Some masks have vents on them—these only protect you, not others, because they don’t filter what you exhale!
- Masks that don’t fit properly are much less effective.
- The more layers in a mask, the better it is at filtering droplets, and experts recommend having three layers in a mask.
- Experts encourage the use of filters in masks, as they are likely to shield the wearer from viral particles more.
- Cloth face masks should be washed whenever you return home. You can wash them in a washing machine at the highest acceptable water temperature for the fabric, or hand-wash masks for twenty seconds under hot water with soap, before drying them in a dryer.
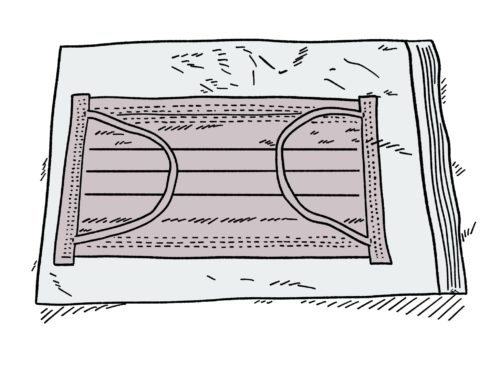
- Surgical masks can be reused but should be thrown out when visibly damaged or soiled. Additionally, you shouldn’t wash them—this will damage their filtering capabilities. Instead, it is recommended to store surgical masks in a Ziploc or Tupperware container for forty-eight to seventy-two hours after use to ensure any viral particles degrade.
COVID: Airborne or Droplet?
- There have been a few COVID-19 outbreaks in which transmission occurred in a way that suggests it can spread as an aerosol, a light particle that can stay in the air for hours. Both the World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC) have thus far not definitively stated that COVID-19 is spread through airborne transmission. In July, after 239 scientists called on the agency to revise its position, the WHO did update its recommendation, saying in part: “short-range aerosol transmission, particularly in specific indoor locations, such as crowded and inadequately ventilated spaces over a prolonged period of time with infected persons cannot be ruled out.”
- Droplet diseases (including strep throat, whooping cough, the flu, and the common cold) travel on respiratory droplets released with coughs, sneezes, and talking. Because of their size compared to air, they usually fall down to the ground and other surfaces quickly and can stay infectious for a long time (several hours for influenza and cold viruses). Airborne diseases (which includes measles, chickenpox, and tuberculosis) are spread on small aerosols that are typically produced by evaporation from respiratory droplets. They can float in the air for minutes to hours.
- Regardless of how the virus that causes COVID-19 travels, wearing a mask and socially distancing have been shown to reduce its spread. If the virus that causes COVID-19 is airborne and spreads through small aerosols, additional caution should be taken in indoor spaces with poor ventilation, where the virus may linger in the air, increasing your chances for infection.
Common COVID Myths Busted
Myth 1: If you test positive for COVID-19, you will have it for life.
It is possible to recover from the disease, and many do. The Chicago Department of Public Health recommends that individuals who test positive seek medical care and treat their symptoms as soon as they can.
Myth 2: If you have recovered from COVID-19, you are now immune and don’t have to worry about getting re-infected.
According to the CDC, there is a lot we don’t yet know about COVID-19 immunity. Individuals who are infected with other coronaviruses usually do not get re-infected in the first few months after they recover, but it is unclear if patients with COVID-19 will experience this level of immunity. There have been reports of a few cases of apparent re-infection, but more information is needed.

Myth 3: 5G technology is linked to COVID-19.
According to the Chicago Department of Public Health (CDPH) and the WHO, 5G technology does not spread COVID-19. The novel coronavirus cannot spread on radio waves or mobile networks.
Myth 4: You can use disinfectant lamps and wands to kill COVID-19.
Possibly some lamps, but only on surfaces and objects (according to the National Academies of Sciences, Engineering, and Medicine). The WHO recommends not using UV-C disinfectant lamps and wands to disinfect any part of your body because UV radiation can damage the eyes and skin.
Myth 5: COVID-19 can spread through wastewater.

According to the CDC, the virus that causes COVID-19 has been detected in untreated wastewater, but researchers do not know if it can cause disease through that route of exposure. So far, there has been no evidence that this has occurred, and the risk of transmission through sewage systems is thought to be low. According to CDPH, the COVID-19 virus has not been detected in drinking water. Conventional water treatment methods that use filtration and disinfection, such as those in most municipal drinking water systems, should remove or inactivate the virus that causes COVID-19.
Myth 6: People with certain blood types are more prone to getting infected with COVID-19.
One study from Harvard Medical School found that individuals who exhibited symptoms who had B or AB blood types and were Rh positive were more likely to test positive for COVID-19, while those with blood type O were less likely to test positive. The researchers also found that patient blood type had no relationship to the severity of COVID-19. However, this is just one study, and more research is needed to understand what is driving these differences.
Myth 7: The best way to prevent COVID-19 is to avoid all meat products and go vegan.

There are several good reasons to go vegan, but thinking that it will prevent COVID-19 infection is not one of them. According to the CDC, there is no evidence that you can get infected by eating food. The main way coronaviruses are thought to spread is person-to-person through respiratory droplets when someone coughs, sneezes, or talks. Before preparing or eating anything, it is important to always wash your hands with soap and water for at least twenty seconds for general food safety.
Long-Term Effects
- The recovery time for people with mild COVID-19 infections that do not require hospitalization is typically between one and two weeks. According to a WHO report on preliminary data of COVID-19 from China in February, people with severe cases of COVID-19 took a median of three to six weeks to recover.
- Recent studies in the US suggest recovery courses can vary a lot depending on age and pre-existing conditions. Age greater than fifty, immunosuppressive conditions, obesity, and chronic kidney disease were most associated with prolonged symptoms. However, even twenty percent of young adults with COVID-19 continued to have some symptoms after three weeks.
- The most common persistent symptoms are fatigue, dyspnea (difficult breathing), cough, joint pain, and chest pain. However, people who become critically ill with COVID-19 may develop persistent difficulties with cognition, mental health, and physical function.
Reopening Chicago
- On May 17, Mayor Lightfoot announced her reopening Chicago plan that enforces and eases restrictions on businesses and citizens depending on trends in COVID-19 case numbers, case positivity (the percentage of positive COVID-19 test results) hospitalizations, deaths, and testing capacity. Currently Chicago is in phase IV, but reinstated some restrictions, such as reducing the number of people allowed in bars and restaurants, in response to elevated daily case numbers on July 24.
- Phase I: Strict Stay at Home: shelter in place, only essential businesses open
- Phase II: Stay at Home: only go outside as needed, wear masks in public
- Phase III: Some non-essential businesses can open if they meet standards; social gatherings of ten or fewer people allowed.
- Phase IV: All businesses can open as long as they meet safeguards; socially gathering allowed up to fifty people indoors, but continue to wear face masks and practice social distancing.
- Phase V: Vaccine is available, non-vulnerable individuals can return to work
- To move to the next phase, Chicago requires a declining rate of new citywide cases over twenty-eight days and/or fewer than 200 new cases per day over fourteen days, positivity rate below five percent, and the capability of testing at least 4,500 people daily. However, since the city is currently in phase IV, it would also require a vaccine to be available to move to phase V.
- If Chicago fails at any of the above criteria, it will reinstate restrictions, or move back to the previous phase.
Vaccination
- At this time, there is no vaccine for COVID-19, and there is too much uncertainty to predict when one might become available.
- Vaccine development happens in three clinical phases, typically over the course of several years.
-
-
- Phase 1: Small groups of people receive the trial vaccine to test things such as safety and appropriate dosage (CDC)
- Phase 2: The clinical study expands—people who have characteristics (e.g., age and physical health) similar to those for whom the new vaccine is intended receive the trial vaccine
- Phase 3: The clinical study scales up—hundreds or thousands of people receive the vaccine to test if it is safe and effective (i.e., does the vaccine reduce the risk of disease for vaccinated people compared to unvaccinated people?)
- The Food and Drug Administration licenses a vaccine only if it is found to be both safe and effective, and if its benefits are found to outweigh any risks. Even after a vaccine has been approved, it continues to undergo testing.
-
- There are currently more than twenty-five COVID-19 vaccine candidates undergoing human trials
- In the Chicago region, two universities have launched initiatives to help test potential vaccines.
- In June, the University of Illinois at Chicago (UIC) called for volunteers for a Phase III clinical trial to test an RNA-based vaccine developed by Moderna, a biotech company, as part of a nationwide study. The National Institute of Allergy and Infectious Diseases is administering the trial. Anyone interested in volunteering to participate in a vaccine trial can register at this website: https://ccts.uic.edu/news-stories/heres-how-to-volunteer-for-a-covid-19-vaccine-trial/. The research team is interested in recruiting a diverse group of participants, including first responders and residents in predominantly Black and Latinx neighborhoods.
- On July 27, Northwestern Medicine announced its COVID Prevention Trials Registry. The registry will connect participants, based on their health profile, to different studies for prevention of the disease. Northwestern University is looking to recruit individuals who are eighteen or older and who live or work in places that put them at a high risk of exposure to COVID-19, such as health care workers, public transportation employees, and individuals living in congregate settings. The research team is also looking for participants from communities that have been disproportionately affected by COVID-19, especially the elderly, Black and Latinx residents, and individuals with underlying health conditions. A Phase III clinical vaccine trial is expected to launch at Northwestern this month. Researchers will test two doses of a vaccine developed by the biopharmaceutical company AstraZeneca and the University of Oxford: one dose to start, followed by another dose a month later. Anyone interested in learning more about or participating in the study can email nuvaccinestudy@northwestern.edu or call (312) 695-5012.
- Dr. Karen Krueger is the principal investigator for Northwestern’s COVID-19 registry. In an email, Krueger said it is difficult to predict when a vaccine might be ready, but she is hopeful that one will be ready by 2021.
Chicago COVID Timeline
- 1/24 – First confirmed case in Illinois, the second case in the US.
- 2/29 – Third confirmed case in Cook County.
- 3/16 – First Chicago death: Patricia Freison, 61-year-old retired nurse from Auburn Gresham.
- 3/18 – Chicago “Shelter-in-Place” order enacted, which encouraged people who are ill to stay at home and self-quarantine.
- 3/26 – Chicago “Stay at Home” Order Enacted, closing parks, beaches, and trails, prohibiting gatherings of more than ten people, and requiring people to stay six feet away from each other.
- 3/27 – US passed Coronavirus Aid, Relief, and Economic Security (CARES) Act. Chicago received $1.1 billion.
- 4/1 – Chicago has performed 18,439 tests, with 3,123 confirmed cases and ninety-nine deaths (mortality rate 1.3 percent, positivity rate 26.9 percent).
- 4/8 – Cook County Jail is reported to be the largest-known source of COVID-19 infections in the U.S.
- 4/20 – Mayor Lightfoot announces Racial Equity Rapid Response Team (RERRT) to work with Austin, Auburn Gresham, and South Shore, which saw high rates of COVID-19 deaths.
- 4/23 – Chicago highest daily positive case rate (1,473 cases/day).
- 5/1 – 91,607 tests performed, with 22,744 confirmed cases, 1,114 deaths ( mortality rate 4.2 percent, positivity rate 27.5 percent).
- 5/5 – Chicago highest daily death rate (fifty-seven deaths/day).
- 5/8 – Chicago announces “Protecting Chicago” Framework, a Five Phase Reopening Plan (and at the time is in phase II).
- 6/1 – 210,191 tests performed, with 45,912 confirmed cases, 2,156 deaths (mortality rate 4.7 percent, positivity rate 10.5 percent).
- 6/3 – Chicago moves to phase III reopening.
- 6/26 – Chicago moves to phase IV reopening.
- 7/1 – 327,862 tests performed, with 52,569 confirmed cases, 2,531 deaths (mortality rate five percent, positivity rate 3.1 percent).
- 7/2 – Travel restrictions on people traveling from high case-rate states enacted
- 7/15 – Chicago highest daily test rate (10,524 tests/day).
- 7/24 – Chicago reinstates some restrictions (because of increase of daily cases) but remains in phase IV.
- 8/1 – 627,709 tests performed, (23 percent of the population), with 61,447 confirmed cases, 2,787 deaths (mortality rate 4.5 percent, positivity rate 3.8 percent).
*Number of deaths from COVID-19 sourced from the Cook County Medical Examiner’s Office, number of tests and cases from the Chicago Department of Public Health. Positivity was measured by looking at the number of tests completed and number of positive test results in the previous two-week period.
Elora Apantaku is a medical doctor and writer. She last wrote about Chicago’s COVID-19 contact tracing plans. Charmaine Runes is a graduate student at the University of Chicago’s Computational Analysis and Public Policy program. She last wrote about the 1995 Chicago heat wave.